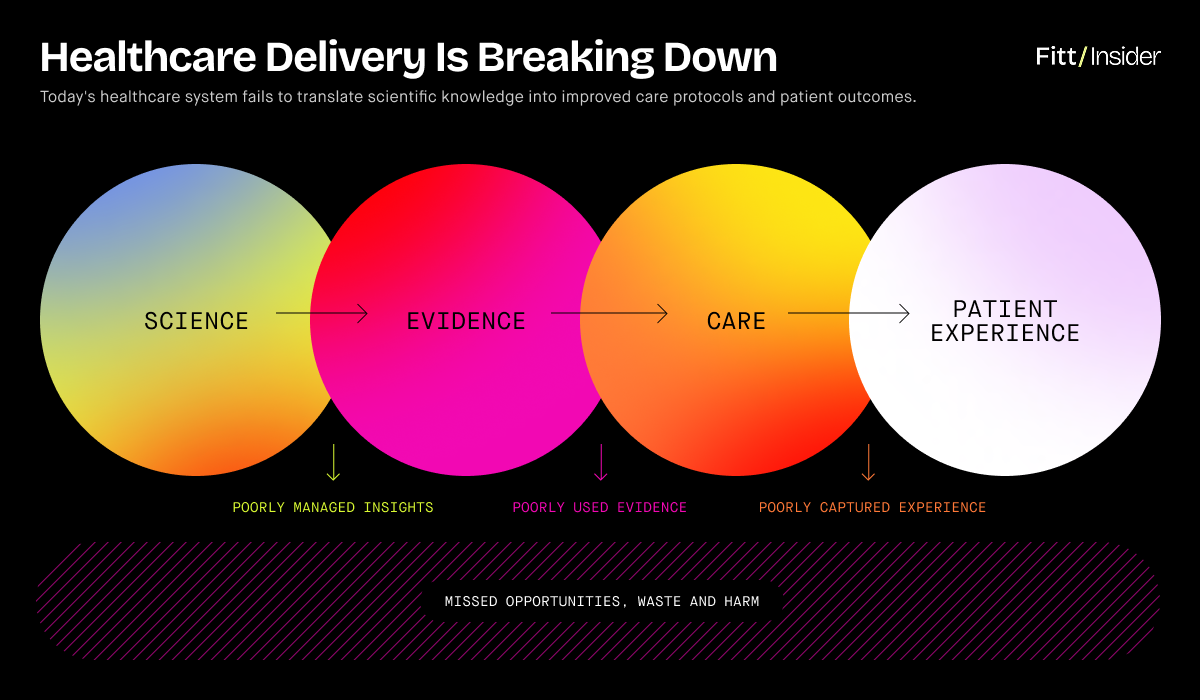
American healthcare is deeply flawed.
Fragmented care, misaligned incentives, and reactive treatments have created the world’s most expensive—and least effective—system.
Heading into Q2 of the 21st century, machine learning is poised to shake things up. Bridging clinical and consumer-led solutions, multimodal AI could unlock an era of high-agency health.
The Future is Now
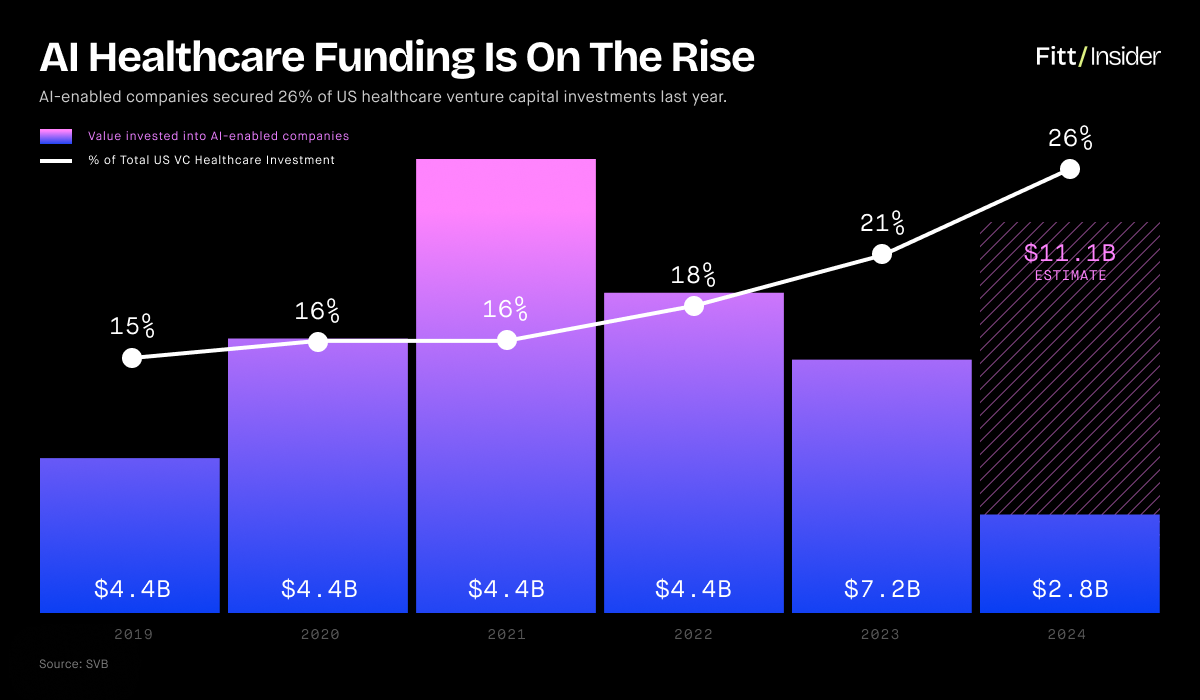
Promising to change the world, AI-driven companies attract a quarter of all healthcare VC dollars. Bullish, investors poured $10.5B into healthcare AI in 2024, with deals growing twice as fast as the broader tech industry.
Encompassing AI-enabled copilots, wearables, biosensors, remote monitoring platforms, advanced diagnostics, and more, the “Internet of Medical Things” market will be worth $167B by 2032.
This report examines AI’s unfolding impact on health and wellness across two distinct areas:
- Clinical Care Journey
- Consumer Health Solutions
Outlining its promises and pitfalls, we explore how new tools could reshape personal and public health management.
Pt. I: Clinical Care Journey
Stretched thin, the US healthcare system is projected to see a shortage of 100K workers by 2028. Meanwhile, admin accounts for up to one-fourth of healthcare costs. AI copilots can solve both.
In 2009, President Obama passed the HITECH Act, digitizing health records to “cut waste, eliminate red tape, and reduce the need to repeat expensive medical tests.”
The bill succeeded in digitizing care—the number of practices using electronic health records (EHRs) jumped ~60% from ’11–’21—but failed to meaningfully integrate data or affect outcomes. Despite spending $29B+ over 15+ years, 97% of hospital data goes unused.
Worse, electronic records added to physician burnout. Moonlighting as admin assistants, PCPs are spending more time on screens and less with patients.
Preventative care is a pipe dream if doctors are overburdened, but GenAI is a game-changer.
Autonomous Copilots
Low-hanging fruit, chatbots and scribes can automate low-risk tasks.
Already in motion, a Stanford study suggests AI can sort and draft messages without sacrificing quality, while Kaiser’s research shows it can redirect a third of doctors’ messages. Infinitely patient, Google claims its LLM even outperforms humans on empathy.
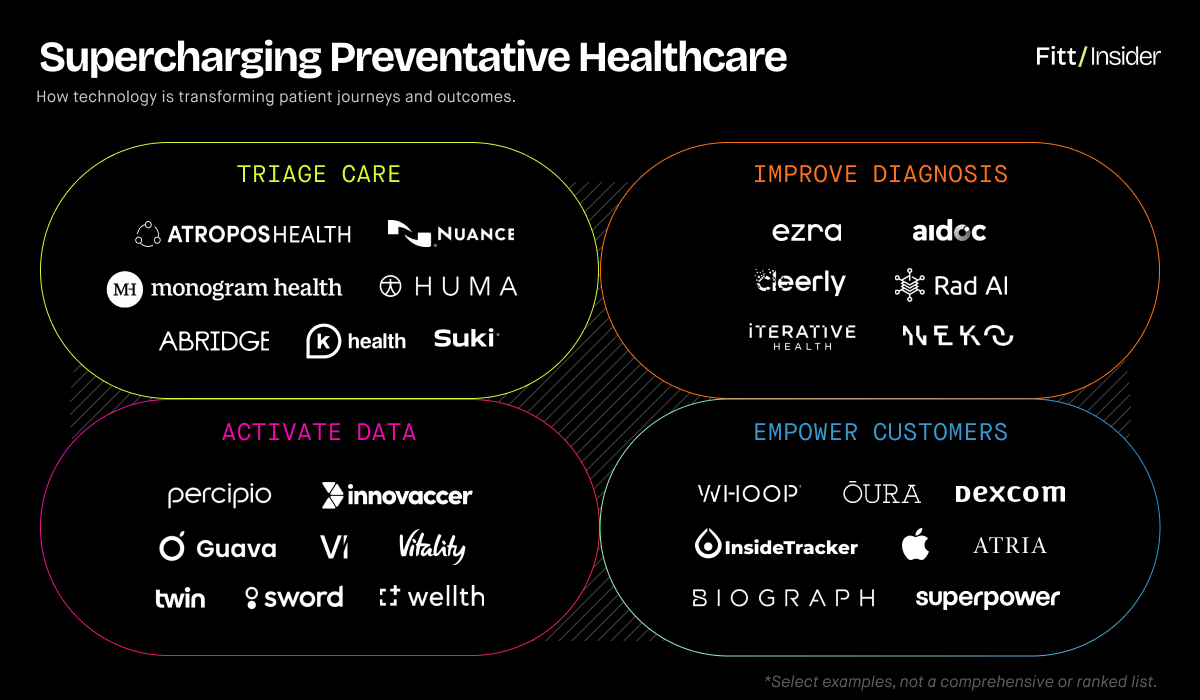
Handling notetaking, ambient scribes from companies like Suki, Nuance, and Abridge let physicians truly listen, with the latter’s 2024 pilot shown to enhance the care experience for docs and patients alike. Clearer notes can also minimize patient handoff mistakes, a contributing factor in 80% of serious medical errors.
A step further, Atropos Health’s ChatRWD acts as a second brain and encyclopedia, combining patient records and real-world data to guide clinical decision-making. Post-visit, Huma’s intelligent remote monitoring platforms help doctors keep tabs from afar, reducing unneeded appointments and readmissions (which cost Medicare $17B annually).
Valued at $1.6B, Hippocratic AI’s agents field follow-up phone calls and simple admin. Creating a 24/7 digital front door, primary care company K Health leverages chat-based agents trained on each patient’s EMR, allowing for personalized virtual support.
Proactive Tools
Advanced medtech and diagnostics can power longevity-focused plans.
In 2022, there were 521 FDA-approved AI/ML-enabled medical devices. Today, there are 950+ spanning radiology, neurology, cardiovascular health, and more. By mid-century, medtech 2.0 could make predictive diagnostics core to routine checkups.
Receiving the FDA’s Breakthrough Device Designation, Cleerly’s machine learning tech turns CT scans into 3D models of the arteries to catch asymptomatic heart conditions. Powering precision GI care, Iterative Health’s AI-assisted colonoscopy device flags colorectal cancer early. Full-suite imaging solutions, Aidoc and Rad AI have partnered with Nvidia and Google, respectively, to speed adoption across major health systems.
Ready for the future, consumers are already opting for out-of-pocket alternatives to traditional care. Longevity-focused proof of concepts, Fountain Life, Biograph, and Atria package IRL clinics, comprehensive diagnostics, expert physicians, and ongoing concierge support for steep membership fees.
The next frontier, digital twin technology x continuous monitoring could give rise to patient avatars, letting doctors predict disease and simulate treatments. Scaling while lowering costs, Q Bio and Neko Health aim to make whole-body scans ubiquitous.
Modern Healers
AI assistance can free physicians to double down on uniquely human insights.
As demonstrated by Forward Health’s failed attempt to fully automate doctor visits, efficiency isn’t everything; people don’t want to be processed by machines but treated by humans.
Case in point, the majority of Americans report wanting docs to ask about mental health, while 57% worry AI will compromise the doctor-patient relationship. A lost art, “narrative medicine” acknowledges the impact of human listening on outcomes, with compassionate physicians seeing higher adherence and better results than detached peers.
If AI helps triage, care teams can give complex cases deserved attention, pursuing root-cause solutions over temporary salves. Building on textbook advice from copilots, doctors can tap experience and intuition to factor intangibles like emotional well-being, spirituality, and mindset.
Respecting the bioindividuality of genetics and social determinants, they’ll “treat the person, not the disease,” as the Father of Modern Medicine Sir William Osler imagined. Put differently, AI can draft plans based on scientific averages; doctors can partner with patients to infuse them with soul. The practitioner’s skill will be knowing what questions to ask.
In practice, this might resemble Monogram Health’s model, where each patient gets at-home tech plus a local, high-touch, multidisciplinary care team attuned to overall quality of life.
Smart Pharma
For issues larger than lifestyle, AI/ML could usher biotech breakthroughs.
Heating up, biotech AI attracted $5.6B in 2024 — almost 3xing YoY. The arms race toward personalized therapeutics and longevity breakthroughs is underway, with huge implications for precision cancer medicine, autoimmune therapies, and more.
Notoriously costly, it takes >$1B and 10 years to bring a drug to market, and 90% of attempts fail. Streamlining the process, the ITIF projects AI could cut pharma R&D costs by $54B/year.
A huge factor, up to 85% of trials fail to recruit or retain participants. Erasing inefficiencies, AI can match diverse patients with appropriate trials plus replace control groups with digital twins. And, if OpenAI x Retro Biosciences succeed, erase aging.
What it means: Overhauling the care journey, partnerships between Mayo Clinic x Google, Mass General x Microsoft, Sutter x GE HealthCare, and more are taking shape. Shifting out of reactive mode, health systems could make “P4 (predictive, preventative, personalized, and participatory) medicine” standard.
Down the line, IRL visits could be less frequent but higher quality, with remote monitoring and holistic plans—spanning food-as-med, exerciseRx, social prescriptions, and pharma—enabling health at home. Selling lifestyle support, fitness and wellness companies could play a more explicit role, with docs offering recs and empathetic oversight.
Pt. II: Consumer Health Solutions
In-person visits will provide a baseline, but patients will need ongoing guidance. A continuation of care, AI can map home wellness routines to amplify adherence and agency.
In the US, 90% of healthcare spend goes toward managing chronic disease. If nothing changes, costs are expected to exceed $9T by 2028.
Lifestyle factors like inactivity, poor nutrition, and substance use cause over half of preventable deaths — pointing to problems of time, access, education, and motivation, not medication.
Unfortunately, just 37% feel empowered by the current healthcare system, while counterforces like Big Food and social media companies spend billions nudging toward bad habits.
In a culture constructed on cheap dopamine, hammering willpower without laying new scaffolding won’t work, but consumer-centric AI might help.
Mission Control Center
To prevent overwhelm, a master hub must translate data from wearables, biosensors, wellness apps, EHRs, and diagnostics into action plans.
Connecting clinical data and real-time biometrics, multimodal AI could inform an all-seeing health optimization dashboard — directly linking lifestyle habits to better outcomes. Emulating the UX of a wealth management robo-advisor, users could enter an end health goal and project likelihood of success based on current habits, adjusting behavior as needed to stay on track.
Playing aggregator, Guava Health’s dashboard is on trend. Extending its brand, Apple could also become the center — transforming its Watches, AirPods, and iPhones into ambient monitors that feed a health super app. For specialized health, wellness, and fitness point solutions, integration with this central hub will be key.
Pushing DTC tests, digital companies like Superpower and InsideTracker already analyze everything from hormones to microbiome and genetics, guiding preventative action. But, marketing to optimizers, their message is lost on more casual wellness consumers.
Palm Pilots
Companion apps can put expert protocols in people’s palms.
Forecasting disease only helps if consumers know what to do next. Adding AI capabilities, wellness companies are 10xing knowledge and support.
A holistic advisor, Oura’s AI delivers personalized guidance on nutrition, rest, training, menstrual cycles, and more. Making clinical inroads, the company linked with Essence Healthcare to give free rings to qualifying Medicare Advantage patients. Meanwhile, Oura partner Dexcom added metabolic health-specific GenAI features to its over-the-counter CGM platform.
For women, Willow’s Ema AI covers topics like breastfeeding and perimenopause, while WHOOP’s Coach specializes in workouts. Catering to families, Panasonic partnered with Aaptiv, Precision Nutrition, SleepScore Labs, Calm, and others for an AI wellness assistant powered by Anthropic’s Claude. Tag teaming, Sam Altman and Arianna Huffington teased a Thrive AI Coach.
Leveraging personal brand, parenting guru Dr. Becky’s Good Inside app includes a chatbot trained on her philosophies, Deepak Chopra duplicated himself to dish AI spiritual advice, and Dexa’s AI pulls from podcasts like Huberman Lab.
Faced with conflicting science, consumers will trust the platform that feels personally relevant, seeking out apps with an attractive UX, active community, and authority on overlooked topics.
A red flag to watch for, as brands hop on the trend, teasing science from pseudo will be tough.
Communities in the Loop
AI will amplify demand for IRL fitness and wellness concepts.
Pitching AI coaches as a behavior change panacea underestimates the human psyche.
The 1% seek concierge treatment because human accountability works and feeling cared for matters. Many Americans know they should eat well and exercise, have access, yet still don’t. More than push notifications, people need to find joy and belonging in new behaviors.
Looking at the rise of social fitness, it’s clear human connection can spark collective lifestyle shifts and solidify healthy self-concepts. Pressured to change by predictive data, people will seek IRL clubs and studios as an extension of care, buying accountability as a service.
Adding an AI feedback loop, Vi’s software applies data science to optimize acquisition, engagement, and retention, predicting members’ behavior to meet them where they are.
Skin in the Game
As data makes progress transparent, outcome-based contracts can fix misaligned incentives.
Taken by the winds of capitalism, private healthcare spiraled into a bonafide “medical industrial complex” in the ’80s. Disincentivizing cash grabs, AI could realign corporate and public profit.
Pioneering a new model, AI-powered MSK platform Sword Health holds itself accountable for outcomes by only charging in full if programs work. With a net ROI guarantee, Spring Health makes a similar promise in mental health. For metabolic health, Twin Health connects tools like CGMs, fitness trackers, and labs to prove the cost-effectiveness of lifestyle medicine vs. GLP-1s.
Adding $275M this year, Innovaccer’s AI healthcare cloud aims to be a one-stop software shop for value-based care, optimizing both business and health outcomes. Landing $20M in January, Percipio Health offers payers and providers a shared platform for managing complex populations — using AI-powered smartphone camera scans to identify patient needs sooner.
Rewarding behavior change, Wellth partners with payers to nudge people toward healthier habits. Tackling the insurance industry, UK-based Vitality and France’s Alan translate lifestyle choices to consumer discounts. Looking ahead, next-gen insurtech could unlock the option of prorated premiums — lowering rates as patients reduce their chronic disease risk.
But safeguards will be important to ensure high-risk populations aren’t financially penalized.
What it means: Moving away from medical paternalism, AI puts patients in the driver’s seat. Transparent, predictive data can demonstrate the value of nonpharmaceutical therapies like diet, exercise, and sleep as a first line of defense, improving consistency and outcomes.
Healthy third spaces could welcome new crowds as people swap habits and find accountability buddies. And given a control hub to connect the dots, more consumers may opt for integrated tech — from strength training machines to smart toilets to diagnostic mirrors and sleep tools.
The Flip Side
Implementing AI won’t come without challenges, from upskilling doctors to redefining liability and securing cross-sector cooperation for quality control.
Left unchecked, AI could be weaponized and privacy compromised for selfish ends. Bringing on Chief AI Officers, health systems like UCSF and Cedars-Sinai are setting rules of governance.
A work in progress, algorithms will have to be continually monitored for accuracy and bias, which requires additional resources. When employed indiscriminately, “off-the-shelf” algorithms can lead to worse outcomes for minorities.
A recent study showed 56% of US hospitals using predictive models had not adequately evaluated for bias, but those that did were typically better funded, suggesting tech could exacerbate quality-of-care divides.
An agnostic technology, AI doesn’t guarantee progress. Like EHRs, it could add noise without improvement unless interoperability is achieved. But when more data means better algorithms, and better algorithms mean more profit, convincing companies to share won’t be easy.
Without goodwill and good policy, we could wind up with a prisoner’s dilemma.
Balance Sheet
America’s Achilles’ heel, healthcare spending accounts for 17.6% of GDP.
McKinsey estimates AI could save the healthcare industry $360B per year, while Brookings projects it could lower the national budget deficit by $900B—roughly one-fifth—by 2044.
The rollout won’t be perfect, and high-profile failures will spark pushback, but measuring AI against perfection is the wrong yardstick. Given the current bar—a sick-care system plagued by burnout, human error, and moral injury—AI should be embraced with guarded optimism.
Creating a “learning health system,” it can improve with each interaction, at the very least reducing repeat mistakes. A caveat, doctors must stay hypervigilant against hallucinations.
Final Thoughts
Widespread adoption of AI across the entire spectrum of care is a matter of when, not if.
Some worry AI will threaten authority, but those concerns should be weighed against its ability to redistribute responsibility. By eliminating barriers to health agency, it unlocks risk-sharing — incentivizing patients, payers, and digital platforms to each play their part in unwinding lifestyle disease. And for the already healthy, it paves the way toward functional, proactive primary care.
Still, as AI adds complexity and chases moonshots, it’s worth considering how much can be solved via subtraction: less lobbying, addictive tech, fast food, workaholism, stress, and toxins.
Even with robo-coaches, well-being will always be an uphill battle until America alters its environmental defaults. Given 80% of health outcomes are owed to social determinants—versus 20% medical care—AI isn’t an excuse to ignore the fundamentals.